UDP-glucose accelerates SNAI1 mRNA decay and impairs lung cancer metastasis
UDP-glucose is the primary cause of morbidity and mortality,and accounts for up to 95% of cancer-related deaths1. Cancer cells often reprogram their metabolism to efficiently support cell proliferation and survival2,3
. However, whether and how those metabolic alterations contribute to the migration of tumour cells remain largely unknown. UDP-glucose 6-dehydrogenase (UGDH) is
a key enzyme in the uronic acid pathway, and converts UDP-glucose to UDP glucuronic acid4 . Here we show that, after activation of EGFR, UGDH is hosphorylated at tyrosine 473 in human lung cancer cells. Phosphorylated UGDH interacts with Hu antigen R (HuR) and converts UDP-glucose to UDP-glucuronic acid, which attenuates the UDP-glucose-mediated inhibition of the association of
HuR with SNAI1 mRNA and therefore enhances the stability of SNAI1 mRNA. Increased production of SNAIL initiates the epithelial–mesenchymal transition, thus promoting the migration of tumour cells and lung cancer metastasis. In addition, phosphorylation of UGDH at tyrosine 473 correlates with metastatic recurrence and
poor prognosis of patients with lung cancer. Our findings reveal a tumour- suppressive role of UDP-glucose in lung cancer metastasis and uncover a mechanism by which UGDH promotes tumour metastasis by increasing the stability of SNAI1 mRNA.
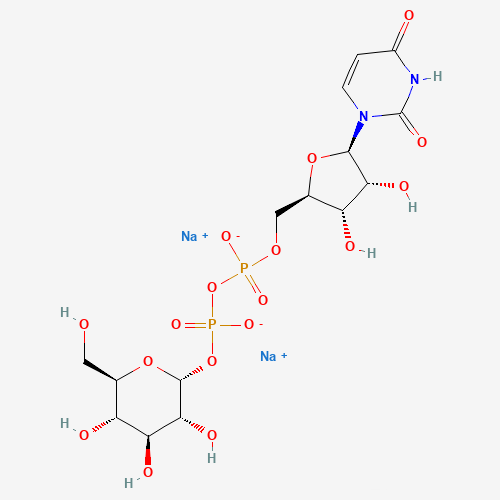
UDP-glucose molecular formula
To identify the metabolic pathway that supports tumour cell migration, we used short interfering RNAs (siRNAs) to knock down 111 rate-limiting enzymes (Supplementary Table 1) or SNAI1 (as the positive control) in human A549 non-small-cell lung carcinoma (NSCLC) cells. Among these enzymes (Supplementary Table 2), UGDH knockdown greatly inhibited tumour cell migration (Fig. 1a and Extended Data Fig. 1a, b; for gel source data, see Supplementary Fig. 1). UGDH
is the key enzyme in the uronic acid pathway that catalyses the conversion of uridine diphosphate (UDP)-glucose (UDP-Glc) to UDP glucuronic acid (UDP-GlcUA) and participates in the biosynthesis of glycosaminoglycans, such as hyaluronic acid (Extended Data Fig. 1c).
Transwell migration assays further supported that UGDH depletion inhibited tumour cell migration and expression of short hairpin RNA (shRNA)-resistant UGDH (rUGDH) fully restored the migration of UGDH-depleted cells, excluding the possibility that this was an off-tar get effect of the UGDH shRNA (Fig. 1b and Extended Data Fig. 1d, e). Moreover, as shown in Fig. 1c and Extended Data Fig. 1f, g, mic that were injected with tumour cells expressing UGDH shRNA devel
oped fewer lung metastases than mice injected with cells expressing a non-targeting shRNA.
The Cancer Genome Atlas (TCGA) RNA-sequencing data of patients with lung adenocarcinoma showed that UGDH mRNA levels were higher in tumour tissues than in normal tissues (Extended Data Fig. 1h) and the levels of UGDH mRNA correlated with the malignancy and prognosis of patients with lung cancer (Extended Data Fig. 1i, j).
The solute carrier-35 D1 gene (SLC35D1) encodes a nucleotide sugar transporter in the endoplasmic reticulum that transports UDP-GlcUA and UDP-N-acetylgalactosamine, which are needed for the biosynthesis of chondroitin sulfate5
. As SLC35D1 was also located on the plasma membrane of A549 and H1299 cells (Extended Data Fig. 2a), we supplemented UGDH-depleted tumour cells that expressed SLC35D1 with UDP-GlcUA. UDP-GlcUA fully restored the reduced cellular UDPGlcUA and hyaluronic acid levels (Extended Data Fig. 2b–d), but only
slightly recovered the decreased migration in UGDH-depleted cells that
expressed SLC35D1 (Fig. 1d and Extended Data Fig. 2e). Moreover,addition of hyaluronic acid (30 μg ml-), which fully recovered cellular hyaluronic acid levels, slightly restored the decreased migration in UGDH-depleted cells (Extended Data Fig. 2f). These results suggest a mechanism in which UGDH is involved in cell migration in addition to promoting the biosynthesis of glycosaminoglycans
The epithelial to mesenchymal transition (EMT) is a process by which epithelial cells lose their cell polarity and cell–cell adhesion, and gain migratory and invasive properties to become mesenchymal stem cells. EMT has been shown in the initiation of metastasis during cancer progression6 . We therefore examined the expression levels of 14 wellknown EMT-related genes and found that UGDH depletion inhibited
the expression of SNAI1 (which encodes SNAIL) and CDH2 (which encodes N-cadherin), but increased the expression of CDH1 (which encodes E-cadherin) (Fig. 1e and Extended Data Fig. 2g–i) SNAIL is a transcription factor that represses E-cadherin but activates N-cadherin to regulate the EMT during embryonic development and cell migration7,8 . It can be regulated at multiple levels, including
transcription, mRNA decay and protein degradation9–11. UGDH depletion did not influence SNAI1 promoter activity (Extended Data Fig. 2j) but decreased the stability of SNAI1 mRNA (Fig. 1f and Extended Data Fig. 2k). Addition of UDP-GlcUA did not restore the decreased stability and expression of SNAI1 mRNA in UGDH-depleted cells (Extended Data Fig. 3a–c). However, either SNAIL overexpression or rSNAIL
expression greatly restored the decreased migration of UGDH-depleted cells (Extended Data Fig. 3d–h), suggesting that SNAIL is the major effector of UGDH in tumour cell migration.
Deregulated epidermal growth factor receptor (EGFR) signalling has a central role in driving lung cancer pathogenesis. Treatment with afatinib, a specific EGFR inhibitor, reduced the stability of SNAI1 mRNA in A549 cells, as determined by mRNA decay assay (Extended Data Fig. 3i, j).
Similarly, EGF increased SNAI1 mRNA stability in a dose-dependent manner (Extended Data Fig. 3k). Notably, UGDH depletion abrogated EGF-increased SNAI1 mRNA stability in NSCLC cells (Extended Data Fig. 3l).
We next investigated how UGDH regulates SNAI1 mRNA stability. HuR was identified to have a strong interaction with UGDH after
